Inaugural T32 Scholars to Explore Inequities in Healthcare
Although cerebral palsy (CP) is the most common motor disorder in babies born preterm, little is known about the early development of impaired motor control function.
“I’ve always been passionate about pediatric medical technology, having studied motor impairments in children and young adults with cerebral palsy,” says Divya Joshi, PhD. “As a research scientist in the biomedical field, I believe it’s critical for our scientific results to have a direct clinical impact. I’m looking forward to conducting this new research that can quickly and directly be translated to clinical care settings.”
Joshi joins postdoctoral fellows Brandon Applewhite, Silvia Karim, and Erika Martinez, as the first cohort of T32 scholars at the NUCATS Institute.
The Institute’s T32 — Equitable TRanslational science to Accelerate Impact of New innovations (E-TRAIN) — is a National Center for Advancing Translational Science-funded training program that seeks to prepare postdoctoral trainees for research careers through mentored research while they develop strategies to anticipate and overcome scientific and operational barriers that impede translation from design through implementation of novel approaches to diagnosis, monitoring, and treatment of human disease. The goal of the program is to prepare early postdoctoral trainees to become leaders in clinical and translational science.
Joshi recently earned her PhD in biomedical engineering at Northwestern. Her doctoral project focused on integrating advanced MRI tools and quantitative biomechanical measurements to characterize the musculoskeletal underpinnings of functional deficits in children and young adults with CP.

As a research scientist in the biomedical field, I believe it’s critical for our scientific results to have a direct clinical impact. I’m looking forward to conducting this new research that can quickly and directly be translated to clinical care settings.”
“After understanding motor impairments that develop following the onset of cerebral palsy, I am excited to shift my research focus to developing early diagnosis and intervention tools for infants at risk for movement disorders,” she says.
The overarching goal of her T32 project will be to develop an accessible, clinically translatable tool that automatically quantifies disrupted motor behavior in prematurely born infants, which will allow for earlier diagnosis and intervention in infants at high risk for movement disorders such as cerebral palsy. Joshi will be mentored by Colleen Peyton, DPT, and James Cotton, MD, PhD.
Knowledge as Power
Like many first-generation Americans, Brandon Applewhite, PhD, was determined to prove himself.
“I’ve always had an interest in the human body, medicine, and academics,” says Applewhite, the son of Jamaican and Trinidadian immigrants. “One of my favorite quotes is from former Emperor of Ethiopia Haile Selassie: In order to make life worthwhile it is also necessary to acquire other things that can only come about after the acquisition of learning.”
After enrolling at the University of South Florida with the intention of going to medical school, Applewhite made what he calls a “whimsical” decision to instead major in chemical engineering.
“Chemical engineering has a manufacturing focus with an emphasis on scalable process and product design which has shaped my approach to biomedical engineering, ensuring that whatever I make in the lab can actually be produced sustainably on a mass scale — in other words, is translational,” says Applewhite, who earned his doctorate in biomedical engineering in 2023 from the University of Miami. “As a PhD, I am still close to the medical field, however my impact is now through the creation of the treatments themselves rather than treating individuals.”
Apart from my scientific goals, I hope to use my research to address racial disparities in vascular disease outcomes by developing patient-specific regenerative therapies and increase diversity in clinical trial recruitment. ”
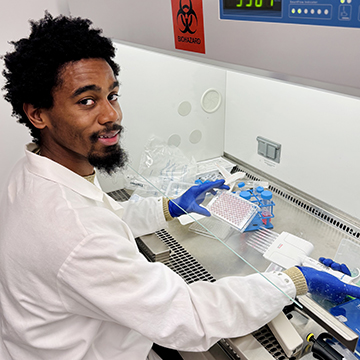
Seeking a career in academia as a scientist and entrepreneur, Applewhite decided to come to Northwestern to do a postdoctoral fellowship in Bin Jiang’s Lab, which is part of the Center for Advanced Regenerative Engineering led by Guillermo Ameer and Feinberg’s Division of Vascular Surgery. It was there that he was exposed to the idea of mitochondria transplantation.
Researchers have shown that mitochondria — responsible for helping power a cell’s functions — can be isolated from healthy tissues and reintroduced to diseased or damaged tissues to preserve their function and prevent cell death.
However, current mitochondria transplantation approaches are not specific or efficient, on top of the many unknowns regarding the safety and fate of transplanted mitochondria. As a T32 scholar, Applewhite’s goal is to improve the translational potential of this treatment by attaching cell and tissue specific peptides — think magnets that have precise 3D structures so they can only attach to things that fit their shape — to the mitochondria to control where they “go” after transplantation, thereby maximizing the therapeutic effect. For his project, he is particularly focused on delivering mitochondria to blood vessels to encourage healing after surgery.
“This T32 award will provide a transformative experience in my academic and professional career as a scientist and biomedical engineer by providing me with formal training in translational science and equipping me with the tools required to be a leader in the field,” Applewhite says. “Apart from my scientific goals, I hope to use my research to address racial disparities in vascular disease outcomes by developing patient-specific regenerative therapies and increase diversity in clinical trial recruitment. I also want to serve as a mentor for the next generation of underrepresented scientists and encourage underserved students to pursue higher education.”
Tapping Into Brain Waves
An estimated one-third of older adults experience delirium, or sudden bouts of confusion, while admitted to the hospital. The profound impact on patients’ lives and significant emotional and physical burden on caregivers, is a reality that Erika Juarez-Martinez, MD, PhD, has experienced firsthand.
“Importantly, up to 40 percent of delirium cases can be prevented with early detection and proper care,” says Juarez-Martinez. “During a recent study, we also found that Spanish-speaking patients are five times less likely to be fully screened for delirium compared to English-speaking patients. Similarly, patients of color are less likely to receive proper assessments, even though they are at greater risk. This highlights an urgent need for better tools to detect delirium equitably and accurately for all patients.”

This T32 award is a pivotal step in my journey to becoming a leader in clinical and translational neuroscience and will position me to apply for a K-award in the near future.”
Juarez-Martinez is a neurologist and neuroscientist from Mexico City whose passion lies at the intersection of patient care and research. She maintains an ongoing focus on advancing understanding of the mechanisms behind neurological disorders to improve patient care.
“My T32 research aims to create new methods that use brain activity (EEG) and video analysis, combined with machine learning and artificial intelligence techniques to detect delirium early and track its progression. By focusing on diverse groups of patients, including those from different racial, ethnic, and language backgrounds, and using methods that do not rely on language, like measuring physiological brain changes in delirium, we hope to make these tools effective for everyone.”
Juarez-Martinez earned her medical degree from La Salle University in Mexico and completed her neurology training at the Universidad Nacional Autónoma de México and the National Medical Center. She then pursued a master’s degree in neuroscience at Vrije Universiteit Amsterdam, supported by the Holland Scholarship and the VU Fellowship Program. What began as a two-year plan evolved into six transformative years, culminating in a PhD focused on the application of advanced EEG analysis to improve the diagnosis and management of neurological and neurodevelopmental disorders.
“This T32 award is a pivotal step in my journey to becoming a leader in clinical and translational neuroscience and will position me to apply for a K-award in the near future,” says Juarez-Martinez. “It will provide me with the resources and mentorship needed to conduct impactful delirium research in Dr. Eyal Kimchi’s lab. At the same time, it allows me to deepen my expertise in clinical neurophysiology and neuronal network analysis, advancing innovative methods to understand the mechanisms behind neurocognitive disorders.”
Exploring Obesity in new Ways
What can zebrafish tell us about obesity? Silvia Karim, PhD, knows they have the capability to help explain a lot.
“My T32 research will focus on developing genetic models of childhood hyperphagia — a feeling of extreme, insatiable hunger — and obesity using zebrafish,” says Karim. “We will use these models to understand the underlying molecular and biochemical mechanisms underpinning obesity.”
A postdoctoral associate mentored by Erica Davis, PhD, in the Stanley Manne Children’s Research Institute at Ann & Robert H. Lurie Children’s Hospital of Chicago and Northwestern University Feinberg School of Medicine, Karim completed her PhD at Indiana University in 2023.
This award links me to an academic and professional community where I can showcase my work and it will place me in a strong position to obtain independent funding and play a leadership role in translational research.”

“Over time, I ‘ve become fascinated by aspects of rare genetic obesity syndromes where I see the potential for my research to make a meaningful difference in understanding obesity in Bardet-Biedl syndrome (BBS), a rare genetic condition in which obesity is a major challenge for families and barrier to quality of life for affected individuals.”
More broadly, Karim aims to combat operational and scientific obstacles that stand in the way of translating innovative methods for human illness monitoring, diagnosis, and treatment from design to execution.
“I’m very happy to be recognized as a T32 Scholar and I feel honored to be a part of such a distinguished program,” Karim says. “This award links me to an academic and professional community where I can showcase my work and it will place me in a strong position to obtain independent funding and play a leadership role in translational research.”
Research reported in this publication was supported, in part, by the National Institutes of Health's National Center for Advancing Translational Sciences, Grant Number T32TR005124. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Written by Roger Anderson




